Introduction
When patients are scheduled for a CT scan, one of the most common questions they ask is: “Is CT scan done empty stomach?” The answer depends on the type of CT scan being performed, whether contrast dye is used, and the area of the body being examined.
At Ace Imaging Centre, we believe patients feel more comfortable and confident when they are well-informed. This guide will explain in detail when fasting is necessary for a CT scan, what happens if you eat before the scan, how contrast material plays a role, and how to prepare for your appointment.

What Is a CT Scan?
A CT (Computed Tomography) scan is a diagnostic imaging test that combines X-rays and computer technology to produce detailed cross-sectional images of the body. It helps doctors detect:
- Tumors and cancers
- Bone fractures
- Blood vessel blockages
- Internal injuries
- Infections or inflammation
- Neurological disorders
CT scans can be performed with or without contrast dye (oral, intravenous, or rectal), and preparation instructions may differ accordingly.
Is CT Scan Done Empty Stomach?
The requirement for fasting depends on the type of CT scan:
| Type of CT Scan | Fasting Required? | Reason |
| CT Scan without Contrast | No | Regular CT scans without dye usually don’t need fasting. |
| CT Scan with IV Contrast | Yes (4–6 hours) | Fasting reduces the risk of nausea or vomiting due to contrast injection. |
| CT Abdomen/Pelvis with Oral Contrast | Yes (6 hours) | An empty stomach ensures better absorption and clearer images. |
| CT Angiography | Yes (4–6 hours) | Helps improve clarity of blood vessel imaging. |
| Emergency CT Scan | Depends on situation | In emergencies, CT can be done without fasting if life-threatening. |
Answer:
Yes, some CT scans need to be done on an empty stomach, especially those involving contrast dye. However, many routine scans can be performed without fasting.
Why Is Fasting Required for a CT Scan?
Doctors may ask you to fast before a CT scan for the following reasons:
- Reduce Risk of Nausea:
Contrast dye can sometimes cause nausea. Having food in the stomach increases the risk of vomiting during or after the scan. - Prevent Aspiration:
If vomiting occurs, fasting lowers the risk of inhaling stomach contents into the lungs. - Improve Image Clarity:
An empty stomach, especially in abdominal scans, ensures that the stomach and intestines do not interfere with the visualization of organs. - Better Contrast Absorption:
Oral contrast works best when the stomach and intestines are empty, giving radiologists clear images.
What Happens If You Eat Before a CT Scan?
If you mistakenly eat before a scan where fasting is required, it may lead to:
- Rescheduling of the scan
- Inconclusive or unclear images
- Increased risk of nausea or vomiting after contrast injection
Tip: Always inform your radiology team if you have eaten before the test. In some cases, the scan can still proceed if the situation is urgent.
How Many Hours of Fasting Are Required?
The standard fasting time before a CT scan with contrast is:
- 4–6 hours before the procedure
- Only small sips of water are usually allowed
- Diabetic patients may receive special instructions regarding their medications and insulin
CT Scan Preparation: Step-by-Step
Here’s what you can expect when preparing for a CT scan:
1. Before the Scan
- Follow your doctor’s instructions on fasting.
- Remove metallic objects (jewelry, watches, belts).
- Inform your doctor about:
- Allergies to contrast dye
- Pregnancy or possibility of pregnancy
- Kidney disease or diabetes
- Current medications
- Allergies to contrast dye
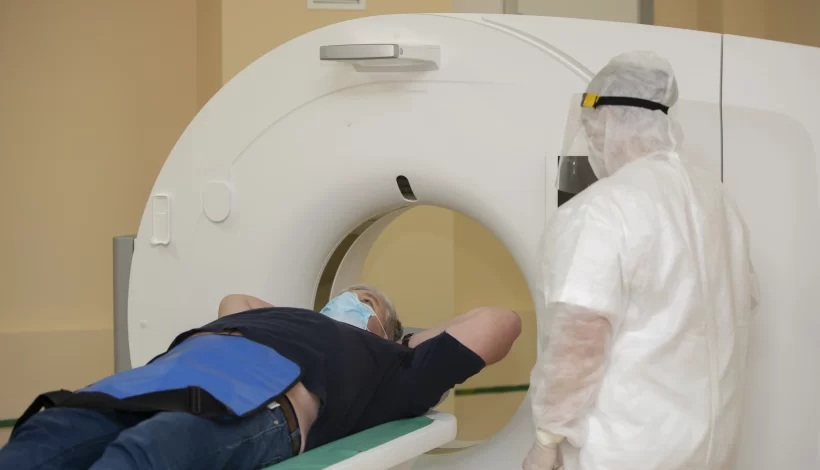
2. During the Scan
- You will lie on a motorized table.
- The table slides into the CT machine.
- If contrast is used:
- IV contrast may cause a warm sensation or metallic taste.
- Oral contrast is usually given 1–2 hours before the scan.
- IV contrast may cause a warm sensation or metallic taste.
- The scan usually takes 15–30 minutes.
3. After the Scan
- You may resume normal diet if no sedation is used.
- Drink plenty of water to flush out contrast dye.
- If you feel allergic reactions (rash, itching, shortness of breath), inform the radiologist immediately.
Special Considerations
1. For Diabetic Patients
- Some medications (like metformin) may interact with contrast dye.
- Patients are advised to stop metformin 48 hours after contrast scans.
2. For Kidney Patients
- Contrast dye may stress the kidneys. Blood tests (serum creatinine) may be required before the scan.
3. For Pregnant Women
- CT scans involve radiation. Unless absolutely necessary, alternatives like ultrasound or MRI may be recommended.
4. For Children
- Children may need fasting, depending on the type of CT scan.
- In some cases, sedation is given to help them stay still.
Frequently Asked Questions (FAQs)
1. Is CT scan done empty stomach always?
No. Only CT scans involving contrast dye usually require fasting. Routine scans without contrast can often be done without fasting.
2. Can I drink water before a CT scan?
Yes. In most cases, small sips of water are allowed even during fasting.
3. How long should I fast before a CT scan?
Usually 4–6 hours. Your radiology team will give exact instructions.
4. What foods should I avoid before a CT scan?
Avoid solid foods, milk, coffee, or juice. Only clear fluids like water may be allowed.
5. What happens if I don’t fast before a contrast CT scan?
The scan may need to be rescheduled, or the images may not be clear enough for accurate diagnosis.
Tips for a Smooth CT Scan Experience
- Arrive early to complete paperwork and preparation.
- Wear loose clothing for comfort.
- Bring medical reports and past imaging results.
- Stay calm and relaxed—the procedure is painless and quick.
- Hydrate well after the scan to flush out contrast dye.
Key Takeaways
- Is CT scan done empty stomach?
- Without contrast: Usually no fasting needed.
- With contrast (oral or IV): Fasting 4–6 hours is required.
- Without contrast: Usually no fasting needed.
- Always follow your doctor’s instructions for the specific type of scan you are undergoing.
- Fasting ensures better safety, clearer imaging, and reduced complications.
- If in doubt, contact your radiology centre before the scan.
Why Choose Ace Imaging Centre?
At Ace Imaging Centre, we provide:
- State-of-the-art CT scan technology for accurate diagnosis
- Patient-friendly guidance on fasting and preparation
- Experienced radiologists and technicians ensuring safety and comfort
- 24/7 support for emergency cases
We ensure every patient feels confident and informed before their scan. If you have questions like “Is CT scan done empty stomach?”, our expert team is here to guide you.
Conclusion
The answer to “Is CT scan done empty stomach?” depends largely on whether contrast dye is involved. For scans without contrast, fasting may not be necessary. However, for abdominal scans, angiography, or any test involving contrast dye, fasting for 4–6 hours is usually required.
At Ace Imaging Centre, we recommend that patients always follow their doctor’s preparation instructions for best results. Being informed about your scan helps reduce anxiety and ensures accurate, safe imaging.